A major obstacle in both clinical treatment and research is hyperprolactinemia, a disorder defined by increased blood levels of the hormone prolactin. From new ways of diagnosing the condition to potential pharmaceutical therapies, this article explores the cutting edge of hyperprolactinemia research. This thorough analysis seeks to illuminate the changing terrain of comprehending and treating this complex endocrine illness by investigating the present difficulties in hyperprolactinemia treatment and the prospective future therapeutic approaches.
Hyperprolactinemia: A Brief Overview
The medical ailment known as hyperprolactinemia is more than just a mouthful; it warrants your attention. Hyperprolactinemia, in its simplest form, is defined as an excess of the hormone prolactin in the blood. And no, it will not cause you to suddenly begin producing milk.
Hyperprolactinemia: how it is defined
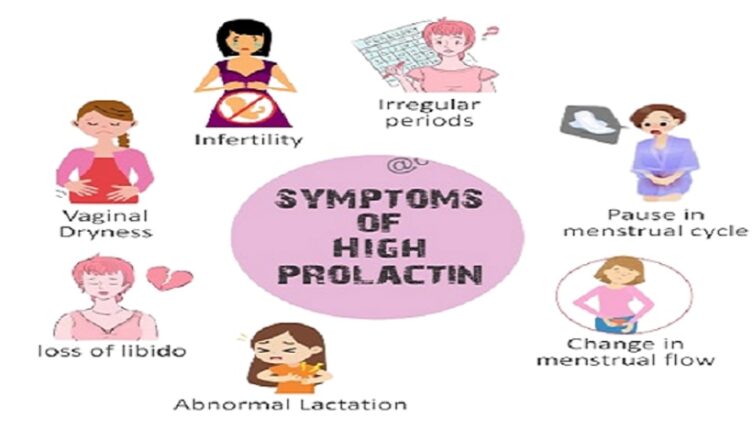
As your body’s method of controlling reproductive function, prolactin is like that buddy who is always trying to make everything neat and tidy. Unpredictable milk production (yes, even in men) and irregular periods are just a few of the symptoms that may arise from an overabundance of prolactin.
Cabergoline is used to treat hyperprolactinemia (high levels of prolactin, a natural substance that helps breast-feeding women produce milk but can cause symptoms such as infertility, sexual problems, and bone loss in women who are not breast-feeding or men). Cabergoline is in a class of medications called dopamine receptor agonists. It works by decreasing the amount of prolactin in the body.
Characteristics and Incidence in Clinical Practice
One study found that hyperprolactinemia affects around 20% of reproductive-aged women, so it’s not as uncommon as you would think. The symptoms might vary from changes in menstrual cycles and breast milk production, which are more noticeable, to less noticeable issues including headaches and eyesight difficulties caused by compression of the pituitary gland.
Hyperprolactinemia: Why It Matters for Researchers
Investigating hyperprolactinemia is like solving a hormonal riddle. Gaining a deeper understanding of this disorder will enable us to create more precise therapies and enhance the lives of those impacted. Making a positive impact on people’s lives is more important than focusing just on the research.
Modern Obstacles in the Treatment of Hyperprolactinemia
Avoiding conventional treatment-related side effects and learning to live with the consequences on a daily basis are just two of the challenges that come with managing hyperprolactinemia.
Consequences of Conventional Medicine
Medication is a common component of conventional hyperprolactinemia therapy, but it is not without risk. Side effects may range from mild to severe, including nausea, dizziness, and even bone density loss. Imagine attempting to resolve a single issue only to unintentionally trigger more complications.
Effects on Welfare
Not only does living with hyperprolactinemia include managing physical symptoms, but it may also take a toll on one’s mental well-being. Envision yourself juggling work, relationships, and self-care while dealing with chronic tiredness, infertility, and other challenges. Nobody volunteered to be a juggler.
Cabergoline 0.5mg is used to treat a variety of illnesses that arise from excessive production of the hormone prolactin. It may be used to treat pituitary prolactinomas, which are tumors of the pituitary gland, as well as certain menstruation issues and issues with fertility in both sexes.
Fresh Methods for Detecting Hyperprolactinemia
The diagnostic landscape for hyperprolactinemia is shifting due to recent developments in imaging and biomarkers.
Technological Progress in Imaging
Modern imaging techniques, such as MRI scans, provide more precise insights into the pituitary gland, allowing clinicians to identify any anomalies that may be causing the excess production of prolactin. Gone are the days of blurry pictures. Better clarity, better decisions—it’s like going from a flip phone to a smartphone.
Early Detection Biomarkers
Hyperprolactinemia is best treated if caught early. Researchers are looking at biomarkers, which are small indicators in bodily fluids like saliva or blood, to identify hormone abnormalities in their early stages, before they cause serious health problems. It’s the equivalent of getting a warning before a storm.
New Pharmacological Approaches to Low Prolactin Levels
Novel pharmacological classes and tailored medicine strategies bode well for the future of hyperprolactinemia therapy.
Different Classes of Drugs and Their Action Mechanisms
Wave farewell to the technique that claims to work for everyone. To better address hyperprolactinemia, new classes of drugs with diverse action mechanisms are being developed. Precision is key, much as when you go from using a general tool to a specialist one.
Prospects for Tailored Healthcare
Why should therapies be standard when no two bodies are identical? When it comes to hyperprolactinemia, personalized medicine entails customizing treatments according to variables such as hormone levels and heredity. Because you are deserving of nothing less, it’s like having a treatment plan tailored to your specific requirements.
The Role of Hormones and Heredity
In an effort to understand how hyperprolactinemia develops, researchers are investigating its genetic basis. One way to have a better grasp of the complex processes involved is to learn how hormones such as estrogen and dopamine control the levels of prolactin.
Neurotransmitters’ Function in Prolactin Release
The intricate relationship between the brain and the endocrine system in hyperprolactinemia may be better understood by delving into the function of neurotransmitters like serotonin and dopamine in prolactin release.
Uncovering Unconventional Molecular Routes
To potentially transform the management of hyperprolactinemia, research into novel molecular pathways paves the ground for the creation of tailored treatments. In order to improve the effectiveness of treatments and decrease their adverse effects, researchers are trying to identify new targets.
Gene and Immunotherapy-Based Strategies
There is hope for targeted and individualized treatments for hyperprolactinemia via immunotherapy and gene therapy. Novel approaches to controlling this endocrine condition have emerged via the use of the immune response and the modification of genetic variables.
How New Technologies Have Influenced Hyperprolactinemia Studies
Researchers in the field of hyperprolactinemia are now able to sift through mountains of data and draw useful conclusions thanks to the combination of big data analytics with artificial intelligence. Making use of these technology improves our knowledge of the disease and speeds up the process of creating individualized treatment plans.
Implementing Telemedicine for the Benefit of Patients
Patients with hyperprolactinemia greatly benefit from telemedicine’s ability to provide remote consultations, monitoring, and assistance, all of which contribute to better patient care. Better patient outcomes are the result of more efficient management made possible by its incorporation, which increases access to expert healthcare services.
Finally, hyperprolactinemia research is always moving forward, which bodes well for better diagnostics, more effective treatments, and better patient outcomes. Hyperprolactinemia management has a bright future thanks to advances in our knowledge of the pathophysiology and the use of technology improvements. There is clear evidence that hyperprolactinemia patients are benefiting from improved care and wellbeing as a result of researchers’ efforts to expand our understanding of the condition and develop new treatments.